Flimsy waiting room chairs.
Waiting rooms plastered with fatphobic magazines, posters and pamphlets.
“One size fits all” blood pressure cuffs, examination gowns and speculums.
And then there is what happens once you are in the healthcare providers office…
Seeking healthcare in a body that does not conform to the thin ideal can be fraught.
So, how do you navigate the healthcare system for weight-inclusive healthcare? Before we get to that…
Why this article shouldn’t need to be written in the first place
A power dynamic exists between healthcare providers (HCP) and patients, where the power is stacked in favour of the HCP and the patient has less, or in some cases, no power.
HCPs are upheld as the ‘expert’ and there can be an expectation that patients fall into line and be subservient; agreeing with everything their HCP says.
Weight bias and weight stigma are also baked into our healthcare system. It means people in bodies that deviate from the thin ideal have snap judgements made about their health status and behaviours (usually negative), leading to assumptions about treatments, medications and further investigations (or lack thereof).
We know from the literature that being subject to weight stigma leads to healthcare avoidance (this is backed up by practice-based evidence and the experiences shared by consumers).
We know from the literature that being subject to weight stigma leads to poorer health outcomes.
Where there is a power dynamic, it should NOT fall to the person with less power to carry all of the labour and responsibility for getting their needs met. Weight inclusive, affirming healthcare SHOULD be the default position, and given that it is not, the onus SHOULD be on HCPs to change.
If affirming, weight inclusive healthcare was the norm, this article would have no reason to exist.
AND, in the absence of this, I hope this piece provides a starting place to consider how you might like your experiences with HCP to go and what type of healthcare you would like to receive.
Some Caveats
This article is not and could never be complete. As much as I have come to understand the pain, frustration and harm of weight stigma in healthcare, both personally and from my clients, this article does lean towards being more generic in nature. This means the nuance of the issue cannot be captured.
It is limited in that it does not accurately capture the complexity of intersecting marginalised identities seeking affirming healthcare (e.g., a larger-bodied First Nations person or a trans person who also has a fat body).
And what has been shared assumes privilege (financial, time etc). This means that some of the ideas might not feel applicable or resonate with you.
Finally, this article has been written based on living and working within the Australian Healthcare System.
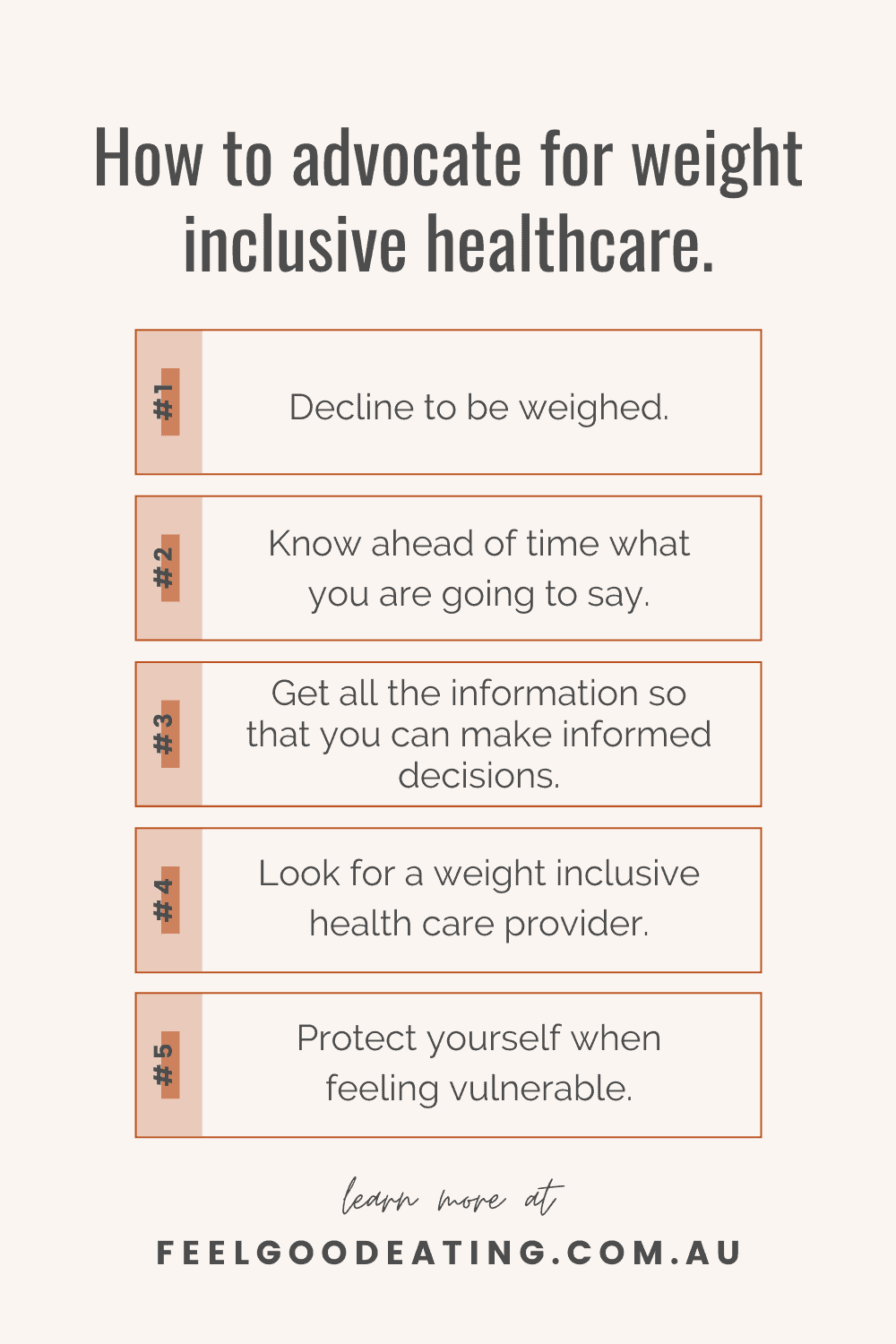
How to advocate for weight inclusive healthcare when…
You are told you need to be weighed
There are a couple of ways you might like to navigate this. You could:
- Decline to be weighed
- Request a blind weight and ask that the number not be disclosed
These suggestions are geared towards accessing weight inclusive healthcare in a primary care setting (e.g., in your doctor’s office) and may not be appropriate in secondary or tertiary care settings (if you are in hospital or undergoing surgery, or if you are being treated for a condition requiring highly specialised care).
ALLY TIP: If you are someone who finds being weighed no big deal, you can decline to be weighed as an act of allyship and culture-making for your fellow humans for whom this is a harmful practice.
You are prescribed weight loss
It can feel like such a kick in the guts to show up to an appointment, lay bare your concerns (if you even get that chance) and what you receive back from your HCP is a prescription to lose weight. To push back on this, one idea for a ‘script’ you could use is:
You: “Do people with smaller bodies than mine also experience X condition?
And when they say yes, because ALL bodies get sick, experience chronic conditions and symptoms, you can ask;
“What would you be suggesting for them?”
When they talk about the options they would offer, you can ask: “Could we try that for me too?”
You are denied treatment (until you lose weight)
Holding treatment, referrals, prescriptions etc. to ransom until you lose weight is unacceptable.
This might be where you want to present your research and evidence that long term weight loss is virtually impossible, causes harm and makes the thing you are seeking treatment for worse over time.
Or, if you don’t have the bandwidth for that, you could ask;
“Ok, but what can I do about X symptom/s in the meantime?”
This question aims to redirect attention back to the symptoms that are concerning you in the here and now. (If you are prescribed weight loss, this could also work as a response and don’t want to use the script above.)
Choice and consent
Being subject to weight stigma in healthcare often takes away our choice and consent.
Choice and consent become another thing that we, as the consumer, end up having to advocate for.
Here’s a couple of examples where this might show up:
Bringing nuance to being weighed:
Rather than flat out declining, Jess Campbell (@haes_studentdoctor) suggests that you might ask what bearing a single weight will have on your care for that consult. She also suggests asking whether a discussion about weight changes (intentional or unintentional weight loss or gain) might provide your HCP with more valuable information for their diagnosis and treatment recommendations. Once you have that information, you might find you are in a better-informed place to decide about declining or accepting being weighed.
Risks and benefits
You can also demand that your HCP lay out the risks and benefits of the intervention or medication or diet they are prescribing.
Ask them what the short- and long-term results and short- and long-term side effects will be. Just like you would expect if you were being prescribed surgery.
Check out Fiona Willer’s Consent for Weight Management Strategy form for an example of what informed consent can look like.
Choosing a provider
Finding a good HCP (whatever ‘good’ means to you) makes navigating the healthcare system and your options for how you want to take care of all facets of your health That. Much. Easier. Some ideas for finding a great provider are to:
- Go by word of mouth
- Ask an HCP you do trust (it might be your podiatrist, your psychologist etc.) if they have recommendations
- Have a look at the providers listed on directories such as HAES Australia and the Association for Size Diversity and Health
- Have a poke around Google to see what the provider’s website is like, what language do they use, how do they show up on social media
- ‘Interview’ them – a weight-inclusive HAES aligned provider will be happy to answer your questions and listen to your concerns (I acknowledge that it might be harder to do with GP/PCP)
- Remember that they are working for you – you can ask more of them, and you can fire them if they do not provide the care you are seeking
Protecting yourself
All of this is to say that you are not obligated to go in and fight every time you see an HCP. Here are some things to consider:
You might not have the energy
Sometimes you might feel ready to speak up, push back and challenge and sometimes you feel too vulnerable. Recognise your own energy, vulnerability and mood and honour that. It is OK and completely understandable if you decide to take a more passive approach in order to protect yourself.
It might not be safe
I had a doctor once share with me that patients need to ‘be nice’ to their HCP because otherwise, they risk the HCP deeming them difficult, a troublemaker and non-compliant (Lindley Ashline shares her experience of exactly that here).
So, while this should never be the case, the reality is, it might not actually be safe to speak up and speak out. The safer option may be to ‘play nice’ to avoid the fallout of speaking up. Because if you don’t get what you need, you might not have the option to see someone else.
Someone else can fight for you
If you have a trusted provider, family member or friend, you might like to ask them if they can advocate on your behalf or come along to the appointment with you for moral support.
Where to go for more
This is by no means an exhaustive list of ways in which you can advocate for weight inclusive healthcare. There are other amazing resources and thoughtful pieces on this topic from people whose voices are much more important than mine. I urge you to check out their writings and advice.
- Ragen Chastain is one of my favourite humans who regularly talks on this topic. Start with:
- More-Love.org Don’t Weigh Me cards
- Nicola Salmon has lots of resources specifically around fertility
- Lindley Ashline regularly writes about weight stigma on her website and newsletter Body Liberation with Lindley Ashline
- This letter from Mosaic Comprehensive Care and Lutz, Alexander & Associates is one you can take with you to support your decision not to be weighed
- If you want to give your provider evidence for why a weight-inclusive approach will be more affirming and health-promoting for you, this article from Lindo Bacon and Lucy Aphramor might be helpful.
I welcome your experiences and suggestions for advocating for weight-inclusive healthcare in the comments below.


 Hi! My name is Nina.
I’m a Certified Intuitive Eating Counsellor taking the ‘diet’ out of Dietitian. I am here to help you reject diet culture, tune into your body’s own inner wisdom about how to truly nourish yourself and ultimately feel good eating™
Hi! My name is Nina.
I’m a Certified Intuitive Eating Counsellor taking the ‘diet’ out of Dietitian. I am here to help you reject diet culture, tune into your body’s own inner wisdom about how to truly nourish yourself and ultimately feel good eating™