Polycystic ovarian syndrome, also known as PCOS, is a complex hormonal condition that is common in people assigned female at birth.
So, what are the most important things you need to know about PCOS? You’ll find them here in this quick guide.
What is PCOS and who experiences it?
The name polycystic ovarian syndrome actually does a really bad job at conveying exactly what PCOS is.
PCOS is considered an endocrine disorder. This means it involves the endocrine system where our hormones are produced and regulated. And because our hormones are important for many different functions in our body, where they are out of balance like they can be in PCOS, it means that PCOS actually impacts the whole body, not just the ovaries and not just the reproductive system.
The hormonal changes often seen in PCOS are increased insulin and increased androgens (a group of hormones that are present in all humans and play a role in the expression of male characteristics).
Statistics and research about PCOS are quite gendered and cite that 1 in 10 or 8-13% of ‘women of reproductive age’ experience PCOS.
However, this does not take into account that people who are non-binary, trans or intersex can also experience PCOS and that PCOS doesn’t resolve or ‘got into remission’ at menopause. People with PCOS might find their reproductive symptoms settle or resolve after menopause but can continue to, or begin to, experience the metabolic effects.
Indigenous, Caucasian European, Asian and North African people are also at higher risk of experiencing PCOS.
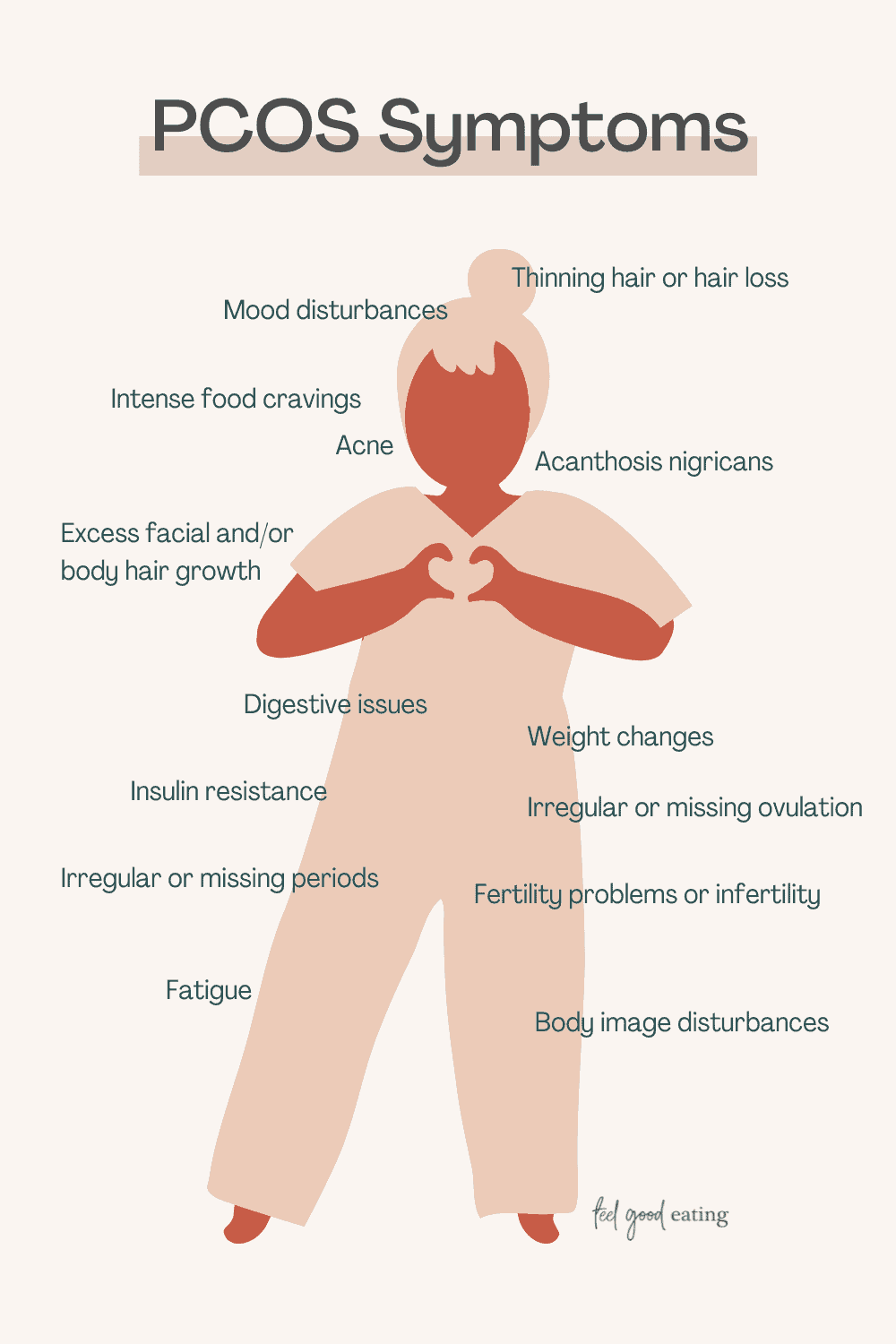
What are the symptoms of PCOS?
The symptoms of PCOS tend to cluster around those related to the reproductive system and those that are metabolic. Symptoms are not just physical, however, but also emotional and mental.
And, not everyone with PCOS is the same, so the types of symptoms and their severity will differ from person to person.
Symptoms can include:
- Irregular or missing periods
- Irregular or no ovulation
- Heavy periods
- Acne
- Thinning hair or hair loss on the head
- Excessive facial and/or body hair growth (hirsutism)
- Fatigue
- Fertility problems or infertility
- Mood disturbances
- Insulin resistance
- Intense food cravings (particularly carbohydrates)
- Body image disturbances
- Weight changes
- Headaches
- Acanthosis nigricans (development of darkened, velvety skin around the neck, armpits, groin)
- Digestive issues
Other co-occurring conditions include:
- Elevated cholesterol
- Non-alcoholic fatty liver
- Elevated blood pressure
- Sleep apnoea
- Depression and anxiety
- Eating disorders
- Type 2 Diabetes
- Cardiovascular disease
- Hidradenitis Suppurativa (or HS)
- Some cancers, like endometrial cancer
- Irritable Bowel Syndrome
What causes PCOS?
At the moment, the exact cause of PCOS isn’t known but research suggests that there is a connection to genetics and family history. Jean Hailes reports that people with PCOS are 50% more likely to have an immediate relative assigned female at birth (e.g., a grandmother, mother, sister etc), who also has PCOS.
How and where we grow up, other family medical history (e.g. Type 2 diabetes), our access to affirming healthcare, exposure to industrial products and agricultural changes in the food system have also been suspected to play a role in the development of PCOS.
And contrary to popular belief, PCOS is not a condition that only affects people with higher weight bodies. Anybody in any type of body can develop PCOS.
How is PCOS diagnosed?
A diagnosis of PCOS can be made if at least two of the following three criteria are met:
- You experience irregular or no periods;
- Elevated levels of androgens are present as determined by a blood test OR you are experiencing acne, excessive hair growth on the face and body and/or hair loss on your head;
- An ultrasound shows that you have polycystic ovaries (polycystic meaning multiple follicles, greater than 20 are visible on one or both ovaries OR the size of one or both ovaries has increased by 10ml)
The process for obtaining a diagnosis should involve a thorough medical, physical and mental health assessment in order to rule out any other conditions like cancers, Cushing’s Disease, hypothalamic amenorrhoea or an eating disorder.
In terms of medical tests, people typically have:
A blood test
Your doctor will be checking a range of biochemical markers and hormones when they order a blood test. In addition to checking androgen levels, doctors will also look at other reproductive hormones like oestradiol (aka oestrogen), follicle-stimulating hormone (FSH)
luteinising hormone (LH). prolactin and might also look at thyroid function, cholesterol, blood glucose and liver function.
An ultrasound
An internal or transvaginal ultrasound provides more accurate results, however, if that is not possible (due to trauma or excessive bleeding), an abdominal ultrasound can be performed.
Note that if you meet diagnostic criteria 1 and 2 above, you don’t need to have an ultrasound.
It’s also important to note that ultrasounds are not indicated for younger people who have had their period for less than eight years.
One final note about the diagnostic process: in order to accurately measure androgen levels, people need to have stopped taking the oral contraceptive pill for at least three months.
What does management involve?
There is no cure, but there are lots of ways in which people can manage living well with PCOS.
‘Lifestyle’
I have put lifestyle options in quotation marks above because lifestyle management for PCOS is a very loaded topic and often subject to weight bias and stigma.
There is no need to pursue weight loss or engage in dieting to manage PCOS. In fact, both of these options are more likely to worsen PCOS and increase the risk of poorer physical, mental and emotional health.
There are many ways in which to approach lifestyle options that are non-diet and weight-neutral.
Lifestyle management involves exploring:
- How you nourish your body
- How you move your body
- Your sleep
- Your stress
- Your mood
- Cosmetic treatments (like skincare, laser, waxing etc.)
Medical
There are a number of medical-based options for managing symptoms of PCOS.
- The oral contraceptive pill is often prescribed as a means to artificially regulate cycles (which is contentious for people looking to treat the root cause of their PCOS). The Pill and other forms of contraception can also be helpful for people who experience excessive bleeding and painful periods (nothing that pain with periods isn’t thought to be due to PCOS)
- A number of medications used in the management of other conditions are often used ‘off label’ to improve insulin resistance, acne, hair loss and excessive hair growth for people who have PCOS
- Antidepressants and anti-anxiety medication might be used to help stabilise and improve mood
Complementary therapies
Complementary therapies include things like supplements, Chinese Medicine and acupuncture.
The permutations and combinations of management options are highly personal and individual. It’s important to talk with a doctor and/or trusted healthcare provider about the different management options so you have all the information before making any decisions. It is also worthwhile knowing that you may have to experiment with a few before you land on what will work best for you and that this may evolve and change over time as you do.
OK, so this was perhaps not as quick a guide as first intended! However, hopefully, the information here has left you better informed and empowered about what PCOS is.
References
https://www.jeanhailes.org.au/health-a-z/pcos/symptoms-causes
Monash University. International evidence-based guideline for the assessment and management of polycystic ovary syndrome. 2018. Melbourne, Australia.
https://juliedillonrd.com/pcosseries2/


 Hi! My name is Nina.
I’m a Certified Intuitive Eating Counsellor taking the ‘diet’ out of Dietitian. I am here to help you reject diet culture, tune into your body’s own inner wisdom about how to truly nourish yourself and ultimately feel good eating™
Hi! My name is Nina.
I’m a Certified Intuitive Eating Counsellor taking the ‘diet’ out of Dietitian. I am here to help you reject diet culture, tune into your body’s own inner wisdom about how to truly nourish yourself and ultimately feel good eating™